by Joseph Giandonato, PhD-c, MBA, MS, CSCS
Once considered just another fat-soluble vitamin that has been long linked to supporting bone health, vitamin D has been lauded as the Swiss Army knife of micronutrients — highly versatile and effective — and now is being hailed as a wonder hormone within the medical community and fitness industry circles.
Deconstructing D
Vitamin D is in fact a steroid. Not the type of steroid that will trigger a positive drug test via gas chromatography-mass spectrometry analysis and warrant a suspension for PEDs, but a steroid in the sense that it regulates gene expression among a wide array of tissues. Technically, Vitamin D is a secosteroid hormone and shares much more in common with fellow endogenous hormones, testosterone and estrogen than its fellow over-the-counter available fat-soluble vitamins, such as vitamins A, E, and K.
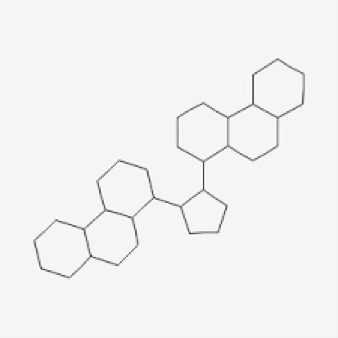
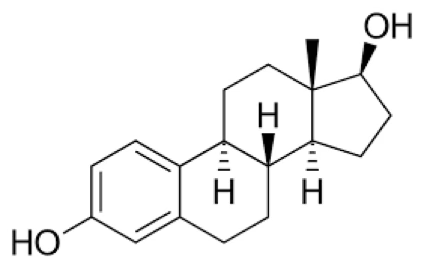
Structurally, Vitamin D bears greater resemblance to testosterone and estrogen than its bottled and ready for sale counterparts as it shares a cyclopentanoperhydrophenanthrene ring structure, or chemical backbone, with the latter two.
Cyclopentanoperhydrophenanthrene
Testosterone

Estrogen
Vitamin D
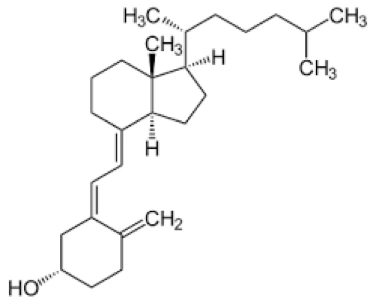
Similar to testosterone and estrogen, Vitamin D is produced endogenously as cholecalciferol, also known as Vitamin D3, and derived from cholesterol. Another version of Vitamin D, ergocalciferol or Vitamin D2, is derived from plant sterols. Both forms of Vitamin D are found in food and dietary supplements for exogenous consumption.
Ultraviolet rays from the sun activate a chemical precursor of Vitamin D, known as 7-dehydrocholesterol to a previtamin form of Vitamin D3 which is transported to the liver and converted to 25-hydroxyvitamin D3 and then shuttled to the kidneys where it is further synthesized into its biologically active form as 1, 25-dihydroxyvitamin D3, or calcitriol.
Exogenous consumption of Vitamin D involves a slightly different metabolic pathway. Ingested Vitamin D is taken up by lipoprotein particles and then absorbed by the lymphatic system prior to entering circulation. At this point, Vitamin D is coursed through the liver and then into the kidneys which result in it being converted into calcitriol.
Versatility of [not a] Vitamin D
Its biologically active form, calcitriol, interacts with target cells throughout the body, namely those within parathyroid glands, dendritic cells, T-cells, keratinocytes, and osteoblasts, and thus presiding over a constellation of body functions, including modulating thyroid functioning, nervous system health, immune system performance, and the integrity of the epidermis, and calcium homeostasis which regulates osteoblastic, or bone-building activity.
Recently, Vitamin D has been shown to be linked to the risk of developing type 2 diabetes (di Filippo & Giustina, 2024) and its role in preventing and treating viral infections has been investigated (Rizwan et al., 2024). Another recent report revealed a potential connection between Vitamin D deficiency and endometriosis (Jennings & Hewison, 2024), a condition characterized by an overgrowth of extrauterine tissue that causes pain and impedes fertility.
In recent years, its neuromodulatory and cardioprotective roles have become clearer. Vitamin D has been shown to impart neuroprotective effects, modulate oxidative stress, and temper inflammation (Gáll, & Székely, 2021). Notably, its role in calcium homeostasis influences calcium signaling (Marambaud et al., 2009), which in turn exerts control of synaptic activity and neurotransmission. Additionally, Vitamin D has been revealed to impede vascular calcifications, a hallmark of atherosclerosis, by way of inhibiting gene expression involved with arterial inflammation (Haider et al., 2023). Further, it has been discovered that Vitamin D is involved with regulating endothelial and vascular smooth cell functioning (Haider et al., 2023) and thus, it could be reasoned that sufficient Vitamin D levels may reduce hypertension and stroke risk. Lastly, Vitamin D levels have been shown to have an inverse relationship with total and low density lipoprotein (LDL) cholesterol and serum triglyceride levels (Haider et al., 2023).
How to Build Your D-fense
Before recommendations related to supplementation are doled out, factors such as sun exposure and dietary patterns must be considered. Moreover, symptoms of low Vitamin D levels are wide-ranging and may include one or more of the following — muscle weakness, compromised immune system functioning, fatigue, depression, and impaired wound healing — which may overlap with numerous conditions. Therefore, definitive measures, such as a routine blood test to measure 1, 25-dihydroxyvitamin D3 levels, are essential to differentiate between a Vitamin D deficiency and something that could potentially be more nefarious.
According to the National Institutes of Health Office of Dietary Supplements (2022), 1, 25-dihydroxyvitamin D3 levels of 50 nmol/L (20 ng/mL) or above are considered adequate for most people for bone and overall health. Levels which deviate considerably below or above may warrant medical intervention. It should be noted that levels may be impacted by the time of year and geographical location as vitamin D levels are lowest during the spring months and among those living above 30 degrees latitude (Giandonato, 2014).
Though ultraviolet rays from sunlight are thought to be superior source of vitamin D production, UV ray absorption can be affected by dark skin pigmentation, time of day, the amount of body surface covered by clothing or sunscreen, and the duration of sun exposure. For individuals who have concerns about their skin or dermatological conditions which can be exacerbated by sun exposure, the dietary pattern should be reconsidered to include more foods containing Vitamin D. Food sources containing significant amounts of Vitamin D include: meat, poultry, beans, and fish — specifically, salmon, tuna, and mackerel). Other sources include egg yolks, mushrooms, organ meats, and fortified dairy products and cereals. Adults aged 18 to 70 years old have a recommended daily allowance (RDA) of 600 IU with a tolerable upper limit intake of 4,000 IU. Supplements containing vitamin D3, which is sourced from animals, possess greater bioavailability than vitamin D2, which is sourced from plants and is not as potent or long acting.
Conclusion
Vitamin D is much more than a vitamin. It is a steroid hormone with immense health fortifying capacity sans the negative connotation of its sex hormone siblings and their derivatives. Per the research, both extant and emerging, Vitamin D lives up to its reputation of being a superhero of sorts as it repels disease and reduces inflammation enabling us to stay healthy and perform better. Before one revamps their diet or clears bottles of Vitamin D from the shelves of their local pharmacy, getting a blood test to ascertain 1, 25-dihydroxyvitamin D3 levels and consulting their physician is highly recommended.
References
di Filippo, L., & Giustina, A. (2024). Vitamin D Deficiency and Type 2 Diabetes: The Dangerous Link Between Two Modern Pandemics. The Journal of Clinical Endocrinology and Metabolism, 110(3), e905–e906. https://doi.org/10.1210/clinem/dgae390
Gáll, Z., & Székely, O. (2021). Role of vitamin D in cognitive dysfunction: new molecular concepts and discrepancies between animal and human findings. Nutrients, 13(11), 3672. https://doi.org/10.3390/nu13113672
Giandonato, J. (2014, November 11). PrimeD to Perform: What Can Vitamin D Do For You? JoshStrength. https://joshstrength.com/2014/11/primed-to-perform-what-can-vitamin-d-do-for-you/
Haider, F., Ghafoor, H., Hassan, O. F., Farooqui, K., Bel Khair, A. O. M., & Shoaib, F. (2023). Vitamin D and cardiovascular diseases: an update. Cureus, 15(11), e49734. https://doi.org/10.7759/cureus.49734
Jennings, B. S., & Hewison, M. (2024). Vitamin D and Endometriosis: Is there a mechanistic link? Cell Biochemistry and Function, 43(1), e70037. https://doi.org/10.1002/cbf.70037
Marambaud, P., Dreses-Werringloer, U., & Vingtdeux, V. (2009). Calcium signaling in neurodegeneration. Molecular Neurodegeneration, 4(1), 20. https://doi.org/10.1186/1750-1326-4-20
National Institutes of Health. (2022). Vitamin D. National Institutes of Health Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/VitaminD-Consumer/
Rizwan, M., Cheng, K., Gang, Y., Hou, Y., & Wang, C. (2024). Immunomodulatory Effects of Vitamin D and Zinc on Viral Infection. Biological Trace Element Research, 203 (1), 1-17. https://doi.org/10.1007/s12011-024-04139-y

Leave a Reply